
During the development of any injectable drug product, drug developers must inevitably answer one critical question: how long will their molecule remain stable after aseptic filling?
The answer has significant strategic implications for every stage of the product’s development cycle and manufacturing process, from the first clinical batches and regulatory submissions, to Phase 3 scaleup and market authorization, to the product’s lifespan. Product stability – and any steps that must be taken to protect it – is a critical component of both the clinical and commercial profile of any injectable medication.
Of course, this question also begs another – how do you know which strategy you need for ensuring your product’s long-term stability, and which dedicated stability program will allow you to put that strategy into action?
Choosing the right strategy for your Products stability

As you formulate your drug product its substance class will provide you with the information on how stable or not it is at room temperature.
Certain groups of molecules have well-known, readily identified stability limits. Several examples include:
- Large molecule biologics, such as proteins, antibodies, and peptides
- Lipid nanoparticles
- Viral vectors
Products based on molecules like those often degrade at room temperature, and thus require additional steps to ensure they remain stable. If your molecule falls into one of these groups, your development team may be able to quickly determine that similar stability considerations may apply. If your product is part of an established or well-characterized substance class, or a biosimilar, related or precedent products can give you a clear indication of which stability strategy may be best for your molecule.
If your drug substance doesn't have comparable products already launched in the market, stability studies conducted during preclinical development will often be the first indicator of any stability limits that may affect a future drug product.
If your product is not stable at room temperature or at 2 to 8°, you need to consider other methods to stabilize the product for long-term storage. For most injectable drug products, the answer is one of three well-established methods – each with its own benefits and drawbacks. Here’s a closer look at each one.
3 key drug stability strategies to consider
Since stability limits are a familiar challenge for injectable drug products, there are three typical solutions to solve the issue.
Each of these three options has advantages and disadvantages, which you and your team will need to weigh when selecting the right approach for your product. Some drug developers may also test two or more options in parallel, choosing the final strategy at a later stage to launch their product. But no matter how you decide to approach this step, you need to start the evaluation and implementation processes as early as possible.
Reformulation: The best option, but often difficult to achieve
For any injectable medication, the optimal stability profile is for the drug product to be stable at room temperature in liquid form. This simplifies and de-risks numerous dimensions of the product’s clinical and commercial lifecycle, including shipping, storage, and expansion into markets with less developed infrastructure.
So, why not reformulate any drug substance with stability limits? Reformulation is a time-consuming and cost-intensive approach, which offers no guarantee of success. It can be an indefinite process that may or may not result in a new formula that delivers reliable stability characteristics – and that adds considerable risk to this approach.
If you are unable to reformulate, there are two other proven options. These approaches also require investment and present their own logistic considerations to work through – but they do deliver predictable stability outcomes for a wide range of injectable drug products.
Freezing: Cost-efficient, but logistically complex and often not applicable
A frozen formulation – if possible – is a familiar method of protecting the integrity of an injectable drug product – one that’s often preferred by drug developers seeking a quick, effective path to the clinic or market. It’s well-established in most regulatory frameworks, and relatively cost-effective – especially compared with an open-ended commitment to reformulation and the relatively cost-intensive process of developing a lyophilization cycle.
But freezing your product also has drawbacks. Not all molecules are suitable to this approach; some are simply too fragile to withstand the multiple freeze-thaw cycles during manufacture. Frozen formulations also require access to a consistent, effective cold chain – a logistically demanding requirement that can complicate distribution channels and limit availability of your product in markets with less-developed infrastructure.
A cold chain can be a major operational complexity for even the most in-demand products. Before committing to a frozen formulation, carefully consider how much of a barrier this requirement may be in the target markets for your product.
Lyophilization: A significant investment in securing long-term stability
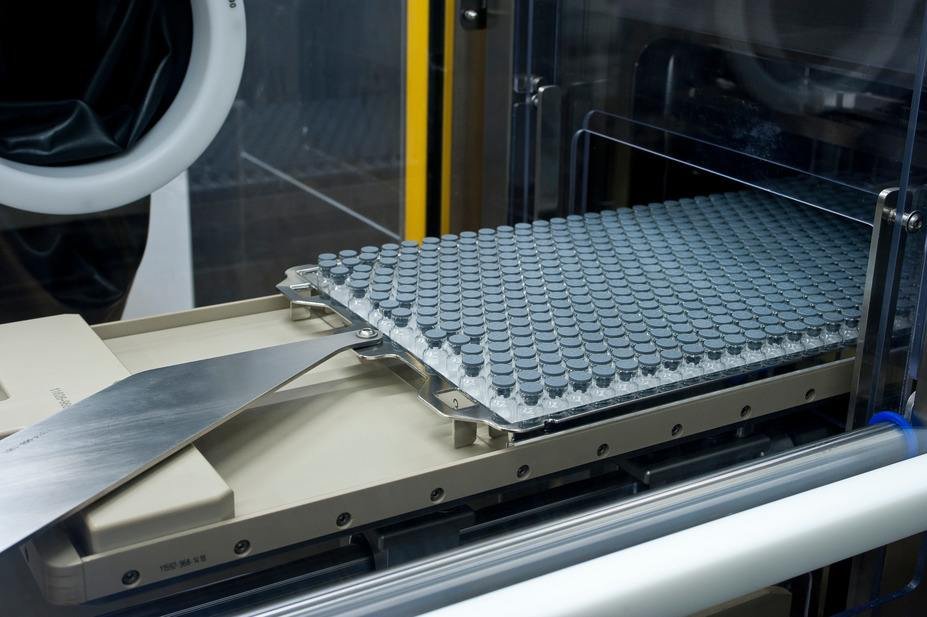
The third stability strategy many drug developers consider is lyophilization: transforming the drug substance into a freeze-dried powder that’s stable at room temperature, and that can be reconstituted as needed.
Like freezing, this method is also effective, proven, and well-established in global regulatory frameworks. Lyophilization, however, is a significantly more complex process that requires additional investment, planning, and lead time to implement successfully:
Operationally, a lyophilization step can’t simply be ‘bolted on’ to your manufacturing processes. Freeze-drying to the standards reflected by cGMP requires a dedicated, customized cycle which must be fully integrated into your aseptic filling process.
Naturally, these steps add development and manufacturing costs to your product, as well as time to your project plans. These need to be factored in as early as possible for best success.
This investment can pay dividends. Lyophilized products typically have a desirable, predictable stability profile, which can be achieved with an approach that balances the consistent success of freezing with the lasting integrity that reformulation seeks to achieve.
Additional stability considerations
In our clinical manufacturing video series, Dr. David Brett, Product and Service Manager at Vetter, discusses each of the three options as well as three key considerations to keep in mind when creating a smart strategy:
- Target markets. The stability plan will depend on whether your company is supplying to many different countries in various scenarios.
- Distribution channels. Is the product going to be widely distributed? This also affects the strategy.
- End-user resources. For example, are there settings where the cold chain isn’t a given? This is critical in determining the best stability plan.
It is also important if the company is considering licensing out the product. Putting a stability strategy in place may add value to the product and enhance future deal potential.
Even if a company is not planning on licensing, choosing the correct approach to stabilizing their product can have a big impact on its market profile.
Interested in more drug stability insights?
Did you find this CDMO Insights post helpful? Dr. David Brett speaks in depth about creating an optimal product stability plan in a how-to video on the Vetter Video Hub. Sign up today to stream this feature and more – including insights on planning your clinical batch and complying with cGMP in your early-stage filling projects.


